Polycystic Kidney Disease is an
autosomal dominant genetic disorder. It is the most frequent cause of renal failure among adults. It is also responsible for 6-8% of dialysis patients in the United States.
Polycystic Kidney Disease is a
multisystemic progressive disorder that is
characterized by the formation and
enlargement of renal cysts in the kidney and other adjacent abdominal organs such as: liver, pancreas, and spleen. It is also
characterized by the bilateral cystic
dilation of the renal tubules, which may lead to end-stage renal disease. Hepatic cysts, cerebral aneurysms, and cardiac valvular
abnormalities are also possible. The disease can be classified either
PKD1 and
PKD2.
PKD1 is expressed as an abnormality in the short arm of chromosome 16.
PKD2 is expressed as an abnormality in the long arm of chromosome 4.
PKD is slightly more severe in males than in females.
PKD symptoms generally increase with age.
The major causes of morbidity is the progressive renal dysfunction, and results in grossly enlarged kidneys and kidney failure.
Over half of patients with
PKD undergo kidney transplant by the age of 60 years old.
Signs/Symptoms:
A decrease in urine
concentration.
HypertensionAbdominal Pain - flank or back: related to kidney enlargement, cystic
enlargement, bleeding,
perinephic hematoma, or urinary tract infections.
HematuriaPalpable bilateral abdominal flank mass
Pallor
Uremic
fetorDry skin
Edema
Testing
Lab Tests such as serum chemistry profile; including calcium and phosphorus, a complete blood cell count, urinalysis, urine culture, uric acid
determination, and intact
parathryoid hormone value.
Ultrasound is the most widely accepted imaging technique for diagnosis of
PKD because it does not use radiation or contrast material. It can diagnosis cysts up 1-1.5cm, as well as detect
extrarenal abdominal features.
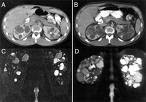
CT scan is a more sensitive imaging
modality because it can detect renal cysts as small as 0.5
cm but because of the use of radiation and contrast material it is not routinely used for diagnosis.
MRI is more sensitive than either ultrasound or CT, especially in determining the difference between
PKD and Renal Cell Carcinoma. It is also the best imaging tool for monitoring kidney size after the patient has undergone treatment in order to assess progress.
Intravenous
Urography (
IVP) was once the most widely used and popular tool for
diagnosing PKD. However, with the evolution of ultrasound,
IVP has been replaced mainly because of its
requirements of contrast material and radiation doses.
Medical Therapy for treatment of
PKDControl Blood Pressure
Use of ACE inhibitors
Control associated disorders
hyperkalemia,
hyperphosphatemia,
hypocalcemia,
hyperparathyroidism, acidosis).
Treat urinary tract infections
Reduce abdominal pain, avoid use of anti-
inflammatory NSAIDSPatients with
PKD and End Stage Renal Disorder may need to undergo
hemodialysis, peritoneal dialysis, or renal
transplantation.
Surgical
Intervention for treatment of
PKDSurgical drainage of infected cysts may be necessary if the infection has not responded to antibiotics. This is often done under the guidance of ultrasound.
Surgical removal of one or more renal cysts for pain management purposes.
Prognosis
PKD patients should maintain a low sodium diet, and avoid any contact sports that would apply direct trauma to the kidney's. These
patient's should have their blood pressure regularly monitored as well as renal ultrasounds every 1-2 years.
PKD1 patients will typically require renal replacement therapy by the age of 53, whereas,
PKD2 patients will usually hold until 68.
http://emedicine.medscape.com/